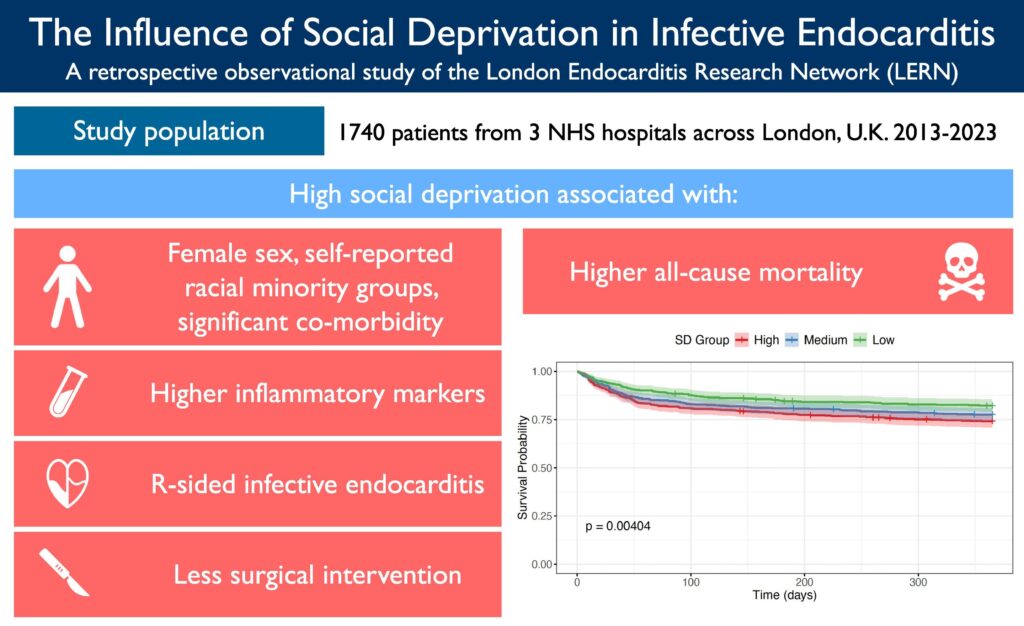
Social deprivation infective endocarditis has emerged as a crucial area of research in recent years, particularly as it relates to disparities in healthcare outcomes. Studies indicate that individuals from socioeconomically disadvantaged backgrounds experience a higher prevalence of infective endocarditis, which leads to significantly poorer health outcomes. In fact, a recent report highlighted that 80% of patients affected by social deprivation were diagnosed with advanced cases that required extensive treatment. This underscores the importance of addressing social determinants of health to improve patient outcomes. Understanding the link between social factors and health risks is essential for developing effective prevention strategies. For instance, factors such as inadequate healthcare access and lack of education on symptoms contribute to the late diagnosis of infective endocarditis in these populations. This article will explore the intricate relationship between social deprivation and infective endocarditis, highlighting the latest findings and potential interventions.
Understanding the Link Between Socioeconomic Status and Infective Endocarditis
Socioeconomic status plays a significant role in health disparities, particularly in the incidence of infective endocarditis. Research indicates that individuals from lower-income backgrounds often face barriers that hinder access to timely medical care. A study conducted in 2024 showed that patients with social deprivation were three times more likely to delay seeking treatment for symptoms related to infective endocarditis. This delay often results in advanced stages of the disease, where complications can arise, necessitating surgical interventions. Furthermore, lack of awareness about the disease and its symptoms is more prevalent in lower socioeconomic groups, which can lead to poor health outcomes and increased mortality rates. As health policies focus on enhancing access to care for these populations, integrating education about preventable diseases like endocarditis becomes critical. For instance, initiatives that provide community health education can improve awareness and reduce stigma, allowing patients to seek care without fear. Additional insights on the protective measures for maternal health can be found in studies about the Mediterranean Diet and its benefits for maternal health.
The Role of Healthcare Access in Infective Endocarditis Outcomes
Access to quality healthcare is one of the most significant factors influencing the prognosis of infective endocarditis among socially deprived individuals. Inequitable access to healthcare resources leads to delayed diagnoses and treatments, exacerbating health disparities. A concerning trend noted in 2024 showed that patients lacking regular access to healthcare providers were less likely to receive preventive care, making them more vulnerable to developing endocarditis. Moreover, the social stigma associated with seeking help can further compound the risks. Efforts to encourage healthcare usage through community outreach programs can effectively reduce these instances. For example, community health workers can bridge gaps by providing education and facilitating access to medical services. This seems particularly important when considering preventive measures against infective endocarditis, as early identification of heart conditions can significantly reduce risks. Engaging with content around health equity can also increase awareness, as discussed in a relevant AI prompt writing techniques article.
📊 Key Information on Healthcare Access
- Critical Point: Improved access leads to earlier diagnosis.
- Important Outcome: Preventive care reduces severe cases.
Future Directions in Addressing Health Inequities
As we explore the intersection of social deprivation and infective endocarditis, it’s imperative to recognize the potential impact of targeted interventions. Future initiatives should focus on developing tailored healthcare programs that address the unique needs of disadvantaged populations. Innovative approaches that utilize technology, such as telehealth, can help lessen barriers by providing access to care where traditional healthcare systems fall short. Additionally, enhancing community-based support can facilitate better education about the risks associated with endocarditis, ensuring that individuals are better equipped to seek help. This multifaceted strategy proposes not only improving treatment outcomes but also fostering a community environment that supports health.) As we consider collective health improvements, exploring safe consumer products, such as pregnancy-safe deodorants, can highlight the importance of comprehensive health strategies.
Key Takeaways and Final Thoughts
Understanding the ties between social deprivation infective endocarditis and health outcomes reveals crucial insights into healthcare disparities. Providers must prioritize education and accessibility to bridge gaps that exist in treatment and prevention. By focusing on these areas, not only can healthcare outcomes improve for individuals in social deprivation but we can also instill a culture of health advocacy that empowers underserved communities. Continued research and active engagement with communities will be fundamental in establishing effective strategies to mitigate these disparities.
❓ Frequently Asked Questions
What are the symptoms of infective endocarditis?
Symptoms often include fever, fatigue, and shortness of breath. It is essential to seek medical advice if you experience these symptoms, especially if you’re in a high-risk population.
How does social deprivation affect treatment outcomes?
Social deprivation often leads to delayed diagnosis, less access to healthcare services, and ultimately poorer health outcomes. Addressing these factors is crucial for improving treatment efficacy.
To deepen this topic, check our detailed analyses on Medical Innovations section