Obesity has increasingly been tied to several serious health issues, yet one of the most concerning facets is its impact on brain health. Recent research highlights that obesity metabolic stress may significantly affect cognitive functions much earlier in life than previously understood. In fact, a shocking statistic shows that young adults with obesity begin to exhibit biological markers indicative of cognitive impairment—similar to those seen in older adults with Alzheimer’s disease. This revelation underscores the importance of addressing obesity metabolic stress to protect both physical and mental health.
Understanding the Link Between Obesity and Cognitive Decline
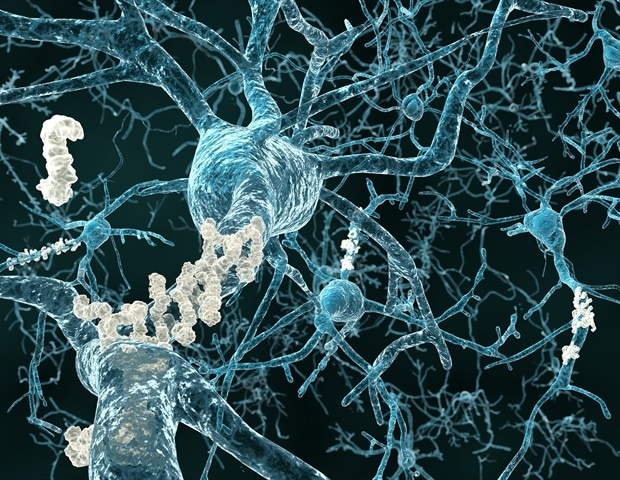
The correlation between obesity and cognitive decline isn’t new. Conditions like obesity, high blood pressure, and insulin resistance place stress on both the body’s vascular and metabolic systems. This stress contributes to accelerating cognitive decline. The study from Arizona State University and its collaborators found troubling indicators; young adults with obesity showed signs of inflammation and early brain cell damage. In particular, there were troublingly low levels of choline, a vital nutrient essential for brain function, which further emphasizes the strain associated with obesity metabolic stress.
Research indicates that chronic inflammation often linked to obesity may pave the way for irreversible cognitive impairment. When individuals are obese, they experience elevated levels of certain proteins and enzymes that indicate stress and cellular damage. These findings strengthen the argument that obesity can etch measurable markers on the brain far before cognitive decline manifests visibly.
The Nutritional Deficiency: Role of Choline
One of the most profound discoveries of this research surrounds the essential nutrient choline. Found in foods like eggs, fish, and leafy greens, choline is crucial for liver health and brain function. With many young adults failing to meet the recommended intake, this deficiency can compound the effects of obesity metabolic stress. The study observed that among individuals with obesity, blood choline levels were noticeably lower, linking this deficiency to increased inflammation and signs of neuron damage.
Interestingly, women exhibited even lower levels of choline compared to men. Low choline levels represent a potential risk factor for cognitive decline, particularly since women are disproportionately affected by Alzheimer’s disease. The nutritional gap here cannot be ignored, as maintaining adequate choline intake could help mitigate the inflammatory response seen in obesity and foster healthier brain function.
Methods and Findings: A Closer Look at the Study
In a meticulous examination, researchers compared 30 young adults—half with obesity and half at a healthy weight. Fasting blood samples were taken to measure various health indicators, including choline levels, inflammatory markers, and neurofilament light chain (NfL), which is a hallmark of neuronal damage. The findings revealed a striking connection: those with obesity not only displayed lower choline levels but also exhibited increased inflammation and neurofilament markers linked to early brain distress.
This pattern is particularly concerning because it suggests that the pathways leading to cognitive deterioration may start decades before traditional symptoms are apparent. As noted by co-author Jessica Judd, ensuring good metabolic health and sufficient choline can significantly influence brain health, potentially laying the groundwork for more resilient cognitive function as we age.
Addressing Metabolic Resilience: Choline and Weight-Loss Treatments
The advent of next-generation weight-loss drugs has revolutionized obesity management but presents a new set of challenges. While these medications effectively promote weight loss and reduce cardiovascular risks, they can inadvertently lead to nutritional deficiencies, including inadequate choline intake. To counteract this, healthcare strategies must adapt to emphasize not only weight management but also the nutritional aspects essential for maintaining metabolic and brain health.
Going forward, research must assess how pairing GLP-1 therapies with adequate dietary choline can support cognitive resilience and overall health during weight loss efforts. This prospective approach can help mitigate the adverse effects of obesity metabolic stress faced by individuals seeking to improve their health.
Conclusion: Building a Healthier Future
Understanding how obesity metabolic stress impacts brain health is crucial in developing effective prevention strategies. Current findings remind us that a balanced diet rich in choline can significantly influence our mental health. As we continue to uncover the long-term effects of obesity, it is essential to foster habits that support both metabolic and cognitive health. This dual approach may pave the way for healthier aging and improved quality of life for future generations.
To deepen this topic, check our detailed analyses on Nutrition & Diet section.
For further insights, explore similar strategies discussed in our analysis of elderberry juice and metabolic flexibility or learn about healthy habits for life transformation.
Moreover, enhancing metabolic health through diet is crucial, as addressed in our detailed discussion about metabolic health diets and its efficacy concerns. Don’t forget to check out practical ideas in our collection of weight loss dinner recipes to kickstart your journey towards a healthier lifestyle.