IBD diagnosis is a critical step in recognizing and managing inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis. Global prevalence is rising, with current data indicating a significant increase in cases among younger populations due to genetic, environmental, and lifestyle factors. In fact, recent studies show that nearly 1.6 million adults in the United States are living with some form of IBD, highlighting the need for precise diagnostic protocols. Understanding the nuances of IBD diagnosis is vital for initiating effective treatment strategies. For more insights into the symptoms and diagnostic techniques, visit the Crohn’s & Colitis Foundation’s diagnostic resources.
Understanding IBD: Symptoms and Initial Assessment
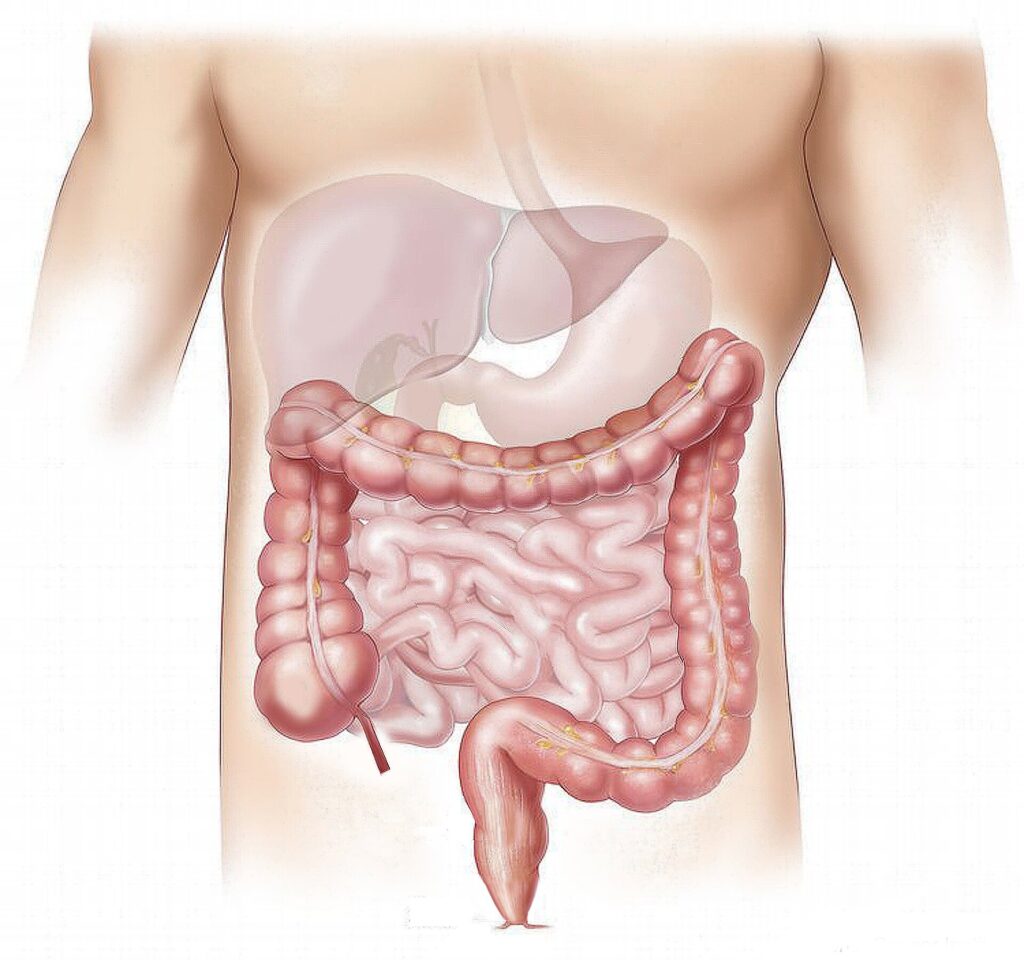
To confirm an IBD diagnosis, healthcare professionals assess various symptoms. Common indicators include chronic gastrointestinal issues like persistent diarrhea, abdominal pain, and rectal bleeding. Additionally, extraintestinal symptoms such as joint pain and skin disorders may also appear. The diagnostic process begins with an evaluation of patient history, followed by physical examinations. According to the Mayo Clinic, further assessments typically involve blood tests to check for inflammation and imaging techniques like MRI or CT scans to visualize intestinal conditions. Early detection is crucial for effective management and can significantly improve a patient’s quality of life.
Diagnostic Techniques for IBD
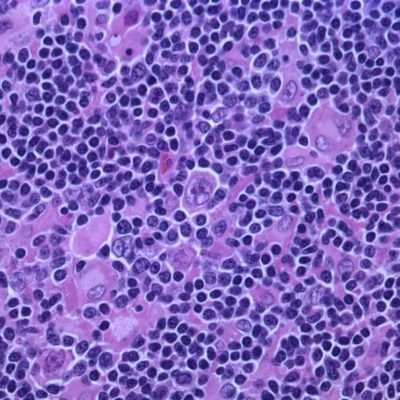
A comprehensive IBD diagnosis utilizes various diagnostic techniques. These may include endoscopic procedures, such as colonoscopy, which allows direct visualization of the intestines and biopsy of suspicious tissues. Endoscopic imaging is essential as it can help rule out other gastrointestinal diseases. Blood tests can reveal inflammatory markers and anemia, common in IBD patients. Additionally, stool tests are performed to check for pathogens and occult blood, enhancing the diagnostic precision. For a deeper understanding of these processes, you can read more on Johns Hopkins Medicine.
📊 Key Diagnostic Techniques
- Colonoscopy: Directly visualizes the intestinal lining.
- Blood Tests: Indicates inflammation and nutritional deficiencies.
- Imaging Studies: Provides detailed pictures of the intestines.
Long-Term Management of IBD Diagnosis
Once an IBD diagnosis is made, long-term management strategies must be established. Treatment plans vary based on the severity and type of disease but usually include medication options such as anti-inflammatory drugs, immunosuppressants, and biologics. Additionally, dietary modifications play a key role; many patients find relief through tailored nutrition plans. Regular monitoring through follow-up appointments is essential to assess treatment efficacy and adjust plans as necessary. Furthermore, patients should be educated on understanding flare-ups and managing stressors that could exacerbate their condition.
Key Takeaways and Final Thoughts
In summary, early and accurate IBD diagnosis is essential for effective management and improved health outcomes. Understanding symptoms, utilizing comprehensive diagnostic techniques, and addressing long-term management strategies are crucial components of care. For more information on the latest in IBD treatments and management, consider consulting resources like Cleveland Clinic for trusted health insights.
❓ Frequently Asked Questions
What are the common symptoms of IBD?
Common symptoms include chronic diarrhea, abdominal pain, fatigue, and weight loss. These symptoms can significantly impact daily activities and require prompt medical attention.
How is IBD diagnosed?
Diagnosis involves a combination of patient history, physical exams, laboratory tests, and imaging studies to accurately identify the presence of IBD and differentiate it from other conditions.
To deepen this topic, check our detailed analyses on Medical Innovations section