In recent observations of critical patients trauma centers, it has become apparent that less than half of the patients requiring immediate transfer actually complete the journey to a specialized facility. This inefficiency can significantly impact patient outcomes, especially in critical situations where timely intervention is crucial. With the rising demand for advanced trauma care, understanding the operational dynamics and transfer protocols is more important than ever. According to the latest studies, timely transfers can enhance survival rates by up to 30%. This article examines the current landscape of trauma care, highlighting the vital factors that influence patient transfers and the disparities in treatment that exist across different regions. For a comprehensive look at how trauma centers operate, check out this resource from the American Trauma Society.
Challenges in Transferring Critical Patients
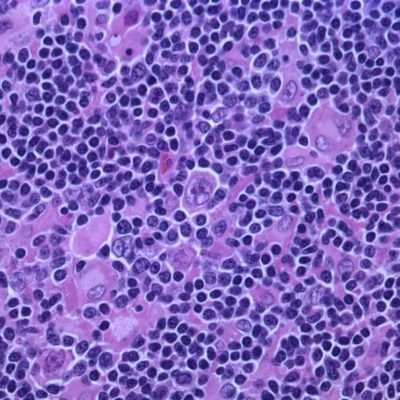
Transferring critically injured patients to trauma centers presents numerous challenges that can hinder effective and timely care. One of the most pressing issues is the lack of appropriate communication between emergency services and trauma centers. For example, studies indicate that poor communication can lead to significant delays, which directly affect patient outcomes. Additionally, logistical issues such as limited transport options or traffic conditions often exacerbate these delays. A significant percentage of patients may not be evaluated by trauma specialists upon arrival, which further complicates their treatment process. In fact, recent data suggests that nearly 40% of trauma patients are overlooked due to system failures. Understanding these operational hurdles is crucial for enhancing patient care within these facilities.
Improving Transfer Protocols in Trauma Centers
Improving transfer protocols is essential to enhance the efficiency and effectiveness of critical patients trauma centers. A data-driven approach has been shown to optimize both patient care and operational workflow. Focusing on the implementation of standardized protocols can significantly mitigate discrepancies in patient evaluations and treatments. Moreover, integrating technology—like real-time tracking and advanced communication systems—can bridge the gaps between emergency responders and trauma facilities. By utilizing such technological advancements, centers will be better equipped to make swift decisions regarding patient transfers. Facilities like the Penn Trauma Centers are already seeing breakthroughs in their patient care protocols through these innovations.
📊 Key Statistics on Trauma Care
- Effective Communication: Critical for successful transfers
- Technological Integration: Key to improving outcomes
- Standardized Protocols: Essential for streamlining care
Patient Outcomes: The Impact of Trauma Center Transfers
The outcomes for patients transferred to critical patients trauma centers can vary widely based on several factors including the level of care provided upon arrival. Research indicates that patients who receive care in a Level I trauma center experience significantly improved survival rates compared to those without specialized attention. For instance, a study published in JAMA Surgery highlighted improved outcomes in patients receiving timely interventions. This underscores the importance of not just transferring patients, but ensuring they are admitted to facilities equipped to handle such critical cases promptly.
Key Takeaways and Final Thoughts
In summary, the landscape of critical patients trauma centers is complex but critical to patient survival. As hospitals and trauma centers strive to improve their processes, addressing communication and operational gaps is paramount. Increased investment in technology and standardized protocols can lead to better patient outcomes and enhanced efficiency. Recognizing the impact of timely transfers cannot be overstated. For further insights into effective trauma care, refer to the Mayo Clinic’s resources.
❓ Frequently Asked Questions
What factors affect patient transfer times?
Several factors, including communication breakdowns and logistical challenges, impact patient transfer times significantly. Ensuring effective collaboration between emergency personnel and trauma centers is essential for timely care.
How can technology improve trauma patient outcomes?
Technology can enable real-time communication and data sharing, ensuring quicker decision-making and better-coordinated care between emergency services and trauma specialists.
To deepen this topic, check our detailed analyses on Medical Innovations section