The human thymus development process is a critical aspect of our immune system, necessary for the maturation of T cells, which play a pivotal role in the body’s defense mechanisms. Recent advancements in the field reveal fascinating insights into how researchers can recreate these processes in laboratory settings using induced pluripotent stem (iPS) cells. Such innovations not only enhance our understanding of thymic organogenesis but also pave the way for potential medical applications in treating immunodeficiencies and improving transplantation outcomes. Research indicates that thymic rejuvenation may become a viable strategy in regenerative medicine, presenting opportunities for enhanced therapies for various diseases.
Recreating Human Thymus Development in the Lab
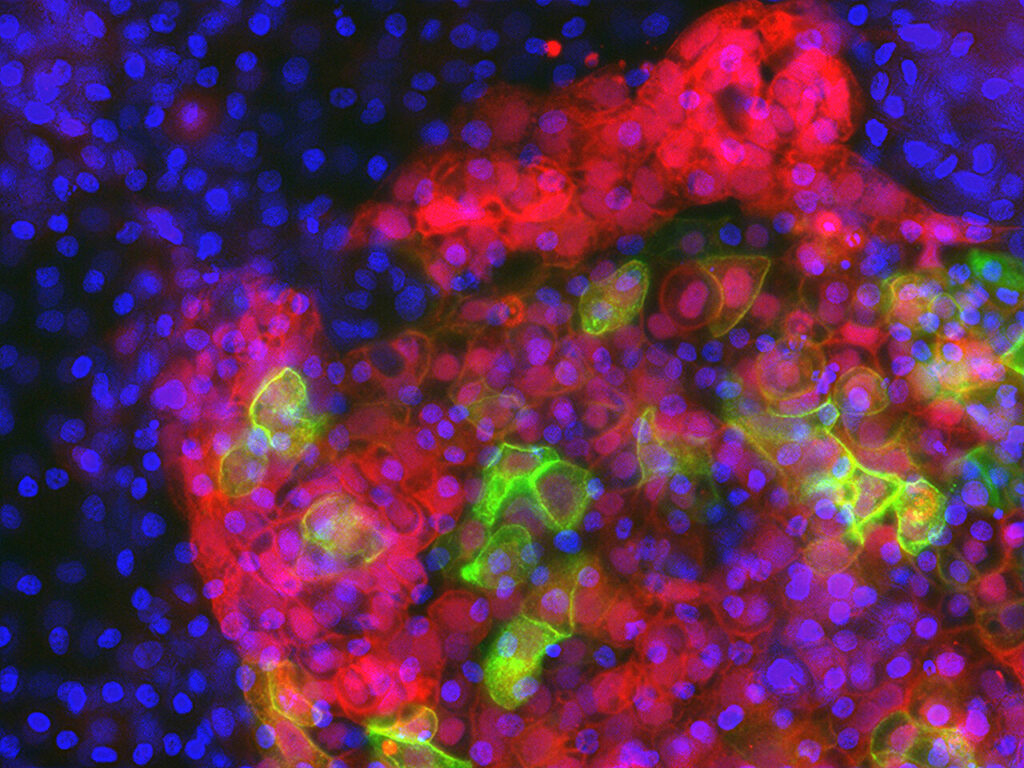
Recent studies have successfully managed to recreate the human thymus development in vitro, utilizing iPS cells derived from adult tissues. This breakthrough allows scientists to examine the intricate cellular interactions that govern T cell maturation. For example, a recent publication reported that researchers utilized cutting-edge techniques to mimic the thymic microenvironment. They achieved this by exploiting 3D culture systems which provide the scaffolding necessary for T cell development. This work is revolutionary, as it not only informs basic science but also has implications in cell therapy and transplant immunology. For more details on the mechanisms involved, see the findings in this Science publication.
Significance of Thymic Development in Immunology
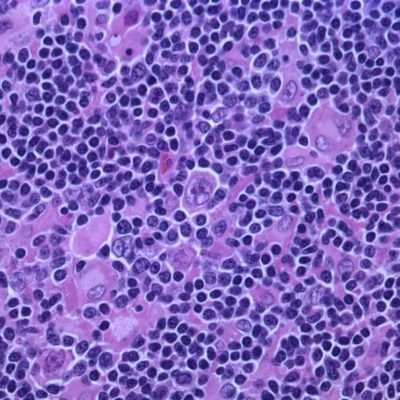
Understanding thymus development is vital because it is integral to establishing the body’s adaptive immune response. In particular, it is within the thymus that T cells undergo selection processes crucial for their functions. The significance of these processes extends to clinical settings—treatments involving stem cells could potentially enhance immune responses in patients receiving transplants. Moreover, recent innovations have highlighted the potential to create patient-specific thymic tissue, which can be developed from their cells. This ability could radically transform the landscape of treatment for congenital immunodeficiencies. Detailed explorations can be found in this article on PubMed Central.
📊 Key Data Overview
- Cellular Milestone: 50-70% of T cells reach full functionality
- Development Timeline: Active between 12 weeks until puberty
Innovations Utilizing Induced Pluripotent Stem Cells
Induced pluripotent stem cells (iPS cells) have beckoned a new era in human thymus development research, offering a pathway to generate functional thymic tissue. Researchers have demonstrated that iPS cells can be effectively directed to develop into thymic epithelial cells, critical for T cell education. The operational efficiency ranges considerably, but advancements in protocol refinement have resulted in significant improvements in output and viability. Such innovations hold promising implications for personalized medicine, particularly for patients with immune deficiencies. Further insights into these groundbreaking studies are available in this Nature article.
Key Takeaways and Final Thoughts
The advancements in recreating human thymus development using iPS cells signal a transformative shift in regenerative medicine. Such technologies not only provide a deeper understanding of thymic function but also promote novel therapeutic avenues for the treatment of immune-related deficiencies. The synergy of scientific inquiry and clinical application underscores the potential of this research to deliver lasting changes in patient care. For additional context on cellular development in immunology, check this Cell Press article.
❓ Frequently Asked Questions
How is the thymus important for T cell development?
The thymus is crucial as it offers an environment where T cells mature and undergo selection, ensuring that only functional cells are released into the bloodstream. This process is vital for effective immune responses.
What role do iPS cells play in research?
iPS cells are pivotal as they provide a renewable source of diverse cell types, enabling researchers to model diseases, study cellular processes, and develop personalized therapies, especially in immunology.
To deepen this topic, check our detailed analyses on Medical Innovations section